By Chidi Oguamanam*
Except perhaps South Africa, credible statistics on the extent of the COVID-19 infection in African countries are lacking. Hypotheses on the rapid degradation of the virus in tropical settings have yet to be proven as COVID-19 ravages the continent. The ongoing upsurge in COVID-19 infections in India and Brazil forebodes an ominous signal for Africa and indeed the rest of the developing world. So far, African countries could not sustain two full months of lockdown. Unlike the rest of the developed world, there were no significant palliatives for ordinary citizens, let alone businesses or corporations. While industrialized countries compute their GDP contraction arising from COVID-19 in the range of 10%, virtually all of Africa is faced with the stark reality of an upwards of 20% drop in their GDP and a total rollback of economic progress of the past two decades. For a continent where over 80% of economic activity is driven by the hand-to-mouth informal sector, continued freezing of economic activity without options would risk political rupture.
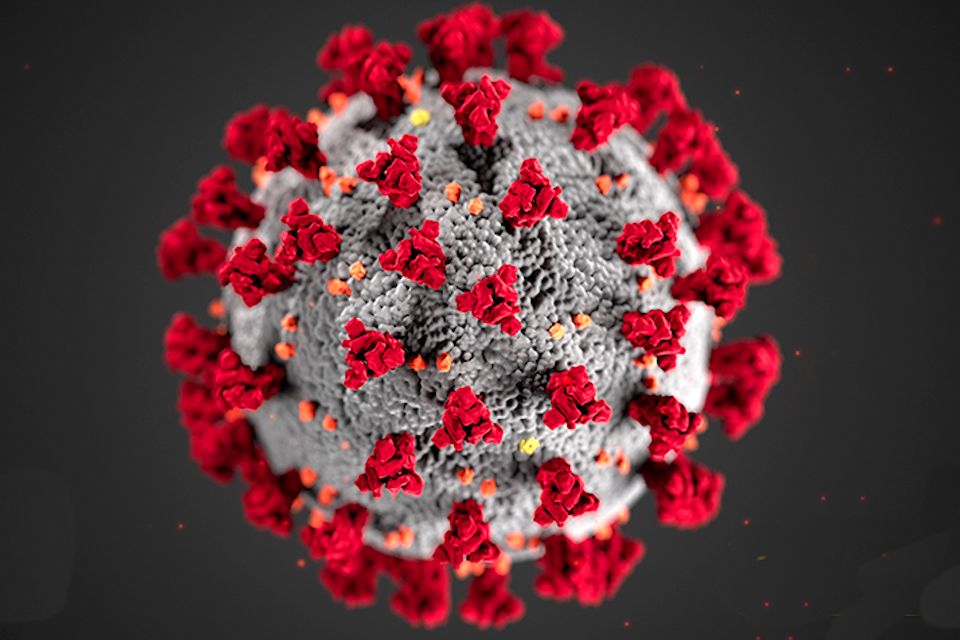
As the world braces up for the second wave of the new Coronavirus, after nearly ten months following the initial outbreak in Wuhan, China, the option of a vaccine offers the hope for a potential return to normalcy. Many countries have invested deeply in the search for viable vaccines. Currently, there are ongoing races for over 150 COVID-19 vaccine candidates of divergent mechanisms, pathways, and platforms, at various levels in the trial process. Vaccinology is a complex enterprise. Its complexity is not only based on its roots in core science. That is a given. In addition, the complexity arises from vaccinology’s obligate interdisciplinary nature. Vaccinology draws together public health, science, ethics, law, public safety, marketing, economics, supply chain management, economic geography and, wait for it, politics.
Investment pathways into vaccines also follow complex structuring and syndication frameworks. For example, such formats include public-private collaborations, exclusive private-sector funded, and even exclusive public R&D initiatives often undertaken by universities and specialized institutions. At the level of this global pandemic, all of these options are on the table. From Germany, China, India, Canada, USA, UK, Switzerland, and counting, there are multiple ongoing collaborations in pursuit of COVID-19 vaccine candidates of various stripes and prospects.
The search for, and production of vaccines, is an expensive exercise. For example, even pending phase three trials, which is the final phase before regulatory approval, many investors go ahead to manufacture millions of vaccines as a hedge betting of a sort. Should such vaccine candidate fail the phase three trial, the investments are ruined for the most part. Where the gamble succeeds, it expedites the introduction of the vaccine into the market, rewarding the investor with a head start. Many of the 150 COVID-19 candidate vaccines are targets for manufacturing at risk, given the prevailing global urgency. However, not many African countries have the financial muscle to flex in this highly expensive endeavour.
Expectedly, as in previous epidemics and associated quests for vaccines, Africa is entering the COVID-19 vaccine race fundamentally disadvantaged. Aside from the governance, infrastructural, fiscal, and R&D deficits, Africa’s major disadvantage in the emerging COVID-19 vaccine landscape lies in what analysts term ‘vaccine nationalism’. It is a tendency by resourceful countries, and even corporations, to prioritize access to vaccines for their countries often arising from sponsored and home-based successful R&D. Aside from exclusive ownership and dispensing of internally manufactured vaccines, vaccine nationalism also involves the inclination of countries to deploy their fiscal muscle to acquire and appropriate viable vaccines for their use from any source money can buy. For example, the United States under Donald Trump has stock-piled over a two years supply of Remdesivir, which has proven efficacious for COVID-19-induced conditions. The medical ethics of vaccinations accords priority access to patients under set guidelines, taking into consideration the most vulnerable and those in direst straits. In most cases, vaccine nationalism is antithetical to medical ethics.
In this US election year, COVID-19 leaves America reeling with the highest death count. The ‘China Virus’, to quote Donald Trump, has dealt a blow on his highfalutin bluster and bombast. Consequently, President Trump’s protectionist ideology takes on a special urgency of a politically expedient nature. In addition to his ongoing blame game with China, Trump has pulled the US out of the WHO, weakening the organization as its number one financier. The latter’s $10 billion-dollar COVID-19 fundraising effort has only managed to reach 10% of the target. A weakened WHO is bad news for Africa and the rest of the developing world, even though WHO’s track record with vaccines in the developing world is not enviable.
With no sensitivity for international solidarity, America’s tentacle is spread all over, internally and externally, in chains of syndications reeking of vaccine nationalism. Agencies like the Biomedical Advanced Research and Development Authority (BARDA), Trump’s Operation Warp Speed initiative, and others are plugged to deliver COVID-19 vaccines to America within uncomfortable proximity of politics and science. Russia’s August 11, 2020 announcement of its approval of the first Coronavirus vaccine will further push Trump’s America to place a political gun on the neck of science. Russia’s “Sputnik V” was rushed into production in under two months of testing on humans. With no credible or robust data, it is one for the Guinness Book of Records. It is sure to further the dangerous mix of politics and science with public safety as a potential casualty. In an era of vaccine skepticism, one can only hope that Russia’s Sputnik V does not offer red meat to vaccine skeptics and conspiracy theorists and thereby undermine ongoing credible COVID-19 vaccine research with longer roll-out timelines.
In these contexts of scientific, political and public health as well as public safety and fiscal uncertainty, Africa finds itself in the scramble for COVID-19 vaccines. Africa’s pathway for timely access to a viable range of COVID-19 vaccine candidates may be limited but not hopeless. Already, the WHO and consortia of countries have endorsed a technology pooling initiative to ensure access to COVID-19 health products for all under a non-exclusive voluntary licensing scheme. Earlier on, since April 2020, Dr. Tedros, the WHO’s Director General, has led the charge in uniting global leaders, researchers, corporations and institutions to ensure that everyone has access to new vaccines, tests, and treatments for COVID-19. This involves creating systems to “standardize assays and standardize regulatory approaches on innovative trial designs and define criteria to prioritize vaccine candidates”. Also, in May 2020, the World Health Assembly issued a COVID-19 Response endorsing a solidarity and collaboration approach to ensure access to all COVID-19 treatment necessities for all. Specifically, the WHA “calls for the universal and timely and equitable access to, and fair distribution of, all quality, safe, efficacious and affordable health technologies and products, including their components and precursors, that are required in the response to COVID-19 as a global priority …”
Africa has many options to leverage on the bargaining power of volume to ratchet centralized vaccine procurement. Given the vacuum in international leadership and a weakened WHO, reputable non-governmental actors in the public health space with deep pockets, such as the Bill and Melinda Gates Foundation, the Wellcome Trust, and GAVI – the Vaccine Alliance, the Global Fund to mention the few, are reliable partners to support Africa access COVID-19 vaccines. Aside from the recent African Development Bank $3b COVID-19 Social Bond, Nigeria’s Dr. Ngozi Okonjo-Iweala, who is also the GAVI Board Chair, has floated the idea of a Global COVID-19 Vaccine Bond as part of humanitarian public health intervention. This is a platform for all stakeholders to pool financial resources together. The idea is to ensure that every country and every person will have access to a sufficient COVID-19 vaccine without financial constraints under a global public good model. Okonjo-Iweala, who also serves with other African Union experts in COVID-19 emergency strategy, rightly believes that African countries should be proactive in seeking out grants and other global concessionary fiscal opportunities to meet their needs for COVID-19 vaccines without further pressuring their precarious financial situation.
All things considered, there is no easy path to access COVID-19 vaccines for Africa. Theoretically, the global vaccine supply for COVID-19 will be targeting about 7 billion people, out of which Africa accounts for 1.2 billion. On a realistic and efficient scale, that will take two to three years to happen. It is also possible that some candidate vaccines could require boosters and other protocols, which will make for a more complicated timeline to reach everyone. In order to secure its interests, Africa must strategically position its institutions in the economic geography of vaccine supply. There are existing institutions within the African Centres of Excellence (ACE) cohorts to serve as hubs that can be retrofitted and plugged into global manufacturing and supply chain. Not only will that mitigate costs, but it would also result in time abridgment, storage, handling, distributional, and dispensing efficiency. And should compulsory licensing of COVID-19 vaccines become inevitable, such institutions will be important collaborators.
If COVID-19 is not stopped in Africa and everywhere, it will undermine all efforts elsewhere. But Africa should not rest on that platitude. Vaccine nationalism is all too real, its logic may not be ethical, but it is politically expedient and compelling. The best Africa can do is remain active in vaccine R&D. For the present COVID-19 reality, Africa needs to prepare and equip its institutional capacities to leverage every opportunity within and without Africa in manufacturing, syndication, or both and in effective participation within the economic geography of the COVID-19 vaccine supply chain.
* Open AIR Steering Committee member and Professor with the Centre for Health Law, Policy and Ethics at the University of Ottawa.